So You Think You Tore Your Meniscus?

Knee pain can happen when least expected.
Whether running, weight training, hiking, or getting out of the car, a misstep or a twist of the knee results in pain and swelling.
Meniscus tears are one of the most common knee injuries, but with proper diagnosis and treatment almost all patients are able to return to their pre-injury activity level.
But, is it a meniscus tear?
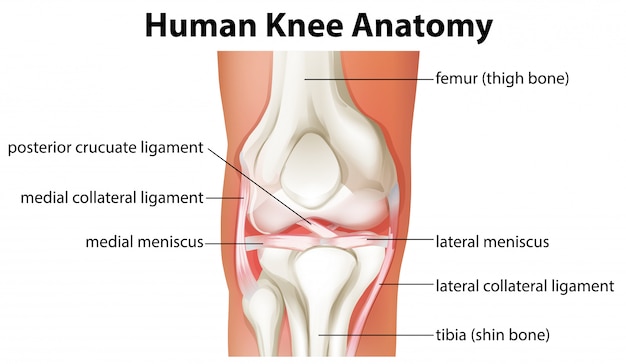
What is a meniscus?
- Two fibrous, wedge-shaped pieces of cartilage
- Located in the middle of the knee joint, between the femur (thigh bone) and the tibia (shin bone)
- Function as shock absorbers for the knee
- Made of tough, rubbery material which also provides stability to the knee joint
How is a meniscus injured?
- Acute injury, often twisting of the knee while partially bent (flexed)
- Degeneration over time related to arthritis
- Leads to weakening of tissue
- Can result in tear from minimal injury such as getting out of car or stepping incorrectly
- Tears are described by location and appearance (i.e. bucket handle, flap, or radial)
What are the symptoms of a meniscus tear?
-
- In an acute tear, a “pop” might be heard or felt, but this is not always the case
- Usually, people are still able to walk on the injured knee and some athletes may even be able to continue to compete despite some pain.
- Some swelling usually occurs within a couple of days
- Causes feeling of stiffness and pressure in knee
- Often enough to limit ability to fully bend and straighten the knee
- Pain is the most common symptom, often localized at the side of the knee where tear has occurred (medial or lateral).
- Catching or locking of the knee may occur if the meniscus tear is unstable or out of position.
- Some report a feeling of instability or the knee giving out underneath them.
What should I expect at physician’s exam?
-
-
- First, your physician will ask you questions about your injury, medical history, and prior knee history
- Physical exam can help to determine if meniscus tear is likely
- Palpation (pushing) on joint lines to determine if painful
- Determination if swelling in the knee joint (effusion)
- Evaluation of range of motion compared to uninjured knee
- Special tests for meniscus tear
- McMurray’s
- Bending and twisting knee to compress meniscus on one side of knee joint and then straightening knee
- Positive test: causes pain in knee and palpable click or catch
- Thessaly’s
- Examiner supports hands of patient to aid in balancing one leg
- Patient bends knee slightly and rotates body on knee
- Repeat testing in increased knee bend
- Positive test: pain and/or locking/catching reproduced
- McMurray’s
-
Do I need an MRI?
If history and exam suggests likely meniscus tear, your physician might order additional imaging
-
-
- X-ray
- Common imaging modality which shows bones well
- Does not show meniscus tissue, but can show other causes of knee pain
- MRI (Magnetic Resonance Imaging)
- 3-D picture which shows soft-tissues including cartilage, ligament, muscles, tendon, and bone
- Often able to show meniscus tear and specify location and type of tear
- X-ray
-
Do I need surgery to relieve my pain?
Choice of treatment depends on the type of tear, size, location and severity of symptoms. Age, activity level, and any related injuries may also affect the treatment plan.
What is non-surgical treatment?
Many meniscus tears can be successfully treated without surgery if symptoms are not persistent and knee is stable without concern for other injury.
-
-
- RICE (Rest, Ice, Compression, Elevation
- Sometimes NSAIDs (Non-steroidal anti-inflammatory) to reduce swelling and pain
- If associated arthritis, degenerative meniscus tear may benefit from knee injection(s)
- Physical Therapy for improved muscle activation and balancing to reduce pain, improve motion, reduce swelling
-
What is surgical treatment?
Persistent pain and mechanical symptoms, instability, or other injuries may indicate a need for surgical treatment.
-
-
- Most commonly a partial meniscectomy
- Done through arthroscopy (camera inserted into the knee joint through small incisions).
- Damaged meniscus tissue is identified and any loose or unstable pieces are removed to prevent recurrent catching and continued symptoms.
- Rarely, meniscus repair may be preformed
- Tear must be in an area with good blood flow (outside third of the meniscus)
- Orthopedic surgeon stitches the torn edges back together.
- Repaired meniscus must be protected from motion and weight bearing in order to allow healing recovery time is longer than from partial meniscectomy.
- After surgery, physical therapy exercises are often recommended to further improve range of motion and to strengthening the knee.
- Most commonly a partial meniscectomy
-
Resources/Additional Information:
MedicineNet. 2020. Knee Joint Picture Image On Medicinenet.Com. [online] Available at: http://<https://www.medicinenet.com/image-collection/knee_joint_picture/picture.htm>
Orthoinfo.aaos.org. 2020. Meniscus Tears – Orthoinfo – AAOS. [online] Available at: http://<https://www.medicinenet.com/image-collection/knee_joint_picture/picture.htm> [Accessed 20 September 2020].
Sportsmedtoday.com. 2020. MENISCUS TEARS | Sports Medicine Today. [online] Available at: http://<https://www.sportsmedtoday.com/meniscus-tears-va-24.htm> [Accessed 20 September 2020].
Photo credits:
Female Athlete Knee Injury <a href=’https://www.freepik.com/photos/background’>Background photo created by freepik – www.freepik.com</a>
Knee Anatomy Graphic <a href=’https://www.freepik.com/vectors/people’>People vector created by brgfx – www.freepik.com</a>